ICSI

Intracytoplasmic sperm injection (ICSI) can be used as a part of an in vitro fertilisation (IVF) treatment to help you and your partner conceive a child. ICSI is the most successful form of treatment for men who are infertile and is used in nearly half of all IVF treatments.
ICSI only needs a few sperms, which are injected directly into the egg. The fertilised egg (embryo) is then transferred to the uterus.
During ICSI the sperm doesn’t have to travel to the egg or penetrate the outer layers of the egg. This means that it can help couples where the man’s sperm:
- can’t get to the egg at all
- or can get to the egg, but for some reason can’t fertilize it.
ICSI is likely to be recommended in the following circumstances:
- A very low sperm count.
- A high percentage of abnormally shaped or slow sperm.
- Sperms that does not show in the fresh sample but can be collected from the testicles or from the duct where sperm is stored (epididymis). This may be needed if your partner has had an irreversible vasectomy or injury.
- Problems with getting an erection and ejaculating, due to spinal cord injuries or diabetes, for example.
- A need to use frozen sperm that is not of the best quality.
- A need to test the embryos to avoid passing on a genetic abnormality.
- In cases that enough eggs are not retrieved, or if eggs retrieved were not fertilized with IVF
- ICSI can also be used to help some couples with unexplained infertility. In this case however, your doctor is likely to initially recommend standard IVF, as ICSI and IVF pregnancy rates are very similar and IVF is a less complex treatment.
How is ICSI carried out?
As with standard IVF treatment, fertility drugs will be needed to stimulate the ovaries to develop several mature eggs for fertilization. Your doctor will use ultrasound, and sometimes blood tests, to monitor this stage of your treatment. When your eggs are ready for collection, you and your partner will undergo separate procedures.
Your partner will be asked to produce a sperm sample himself, by ejaculating into a container on the same day as your eggs are collected.
If there is no sperm in his semen, or he’s unable to ejaculate, it may be possible for your doctor to extract sperm from him through PESA/TESA or TESE surgery.
During egg retrieval, the doctor will remove your eggs using a fine, hollow needle, attached to an ultrasound probe. You may feel a bit bruised and sore after egg retrieval and have some light bleeding.
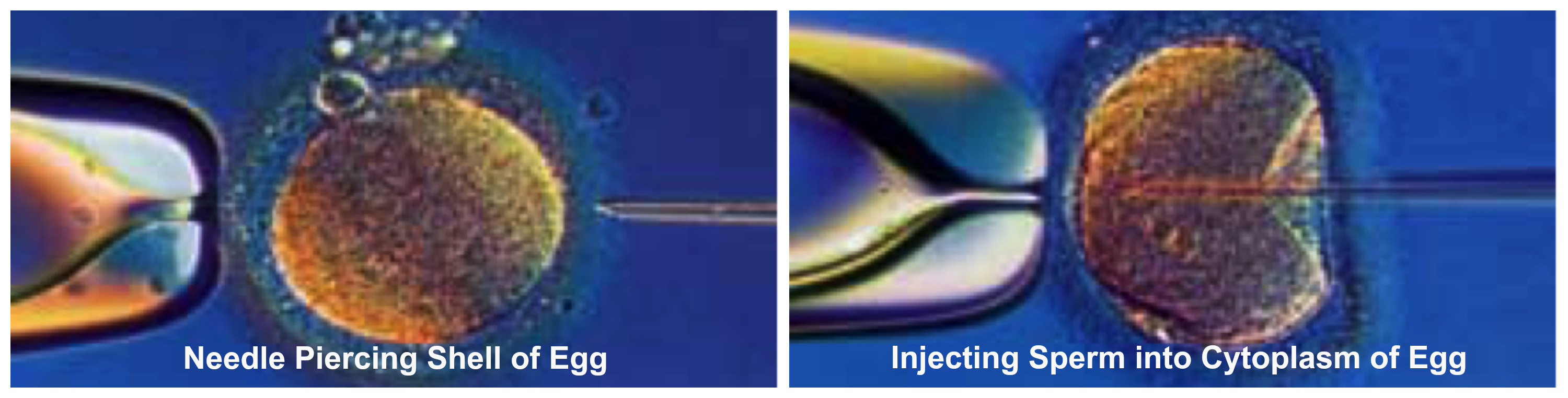
Meanwhile, an embryologist isolates individual sperm in the lab and injects them into your individual eggs. A day later, the fertilized eggs will have become embryos.
The procedure then follows the same steps as in IVF. Your doctor will transfer embryos into your womb, through the cervix, using a fine catheter (tube) usually guided by ultrasound.
Embryos may be transferred two days to three days after fertilization. (The maximum number of embryos that can be transferred to your womb is four.) Good-quality embryos, if there are any, may be frozen in case this cycle isn’t successful or for having another baby in the future. If all goes well, an embryo will attach to the wall of your womb and continue to grow to become your baby. After about two weeks, you will be able to take a pregnancy test.


